 This morning saw the publication of the full and final report from COCAPP. COCAPP has been led by Professor Alan Simpson from City University London, and (as readers of this blog will know) has been concerned with care planning and coordination in community mental health, and the relationships between these processes and recovery-oriented and personalised care.
This morning saw the publication of the full and final report from COCAPP. COCAPP has been led by Professor Alan Simpson from City University London, and (as readers of this blog will know) has been concerned with care planning and coordination in community mental health, and the relationships between these processes and recovery-oriented and personalised care.
Today’s report appears in a single issue of the NIHR’s Health Services and Delivery Research journal. Following the link above takes you to a page from which the complete, 218-page, document can be downloaded. For a shorter read, follow the links instead to either the scientific or the plain English summaries.
Over on the COCAPP blog site, meanwhile, Alan Simpson and Alison Faulkner have written this accessible summary:
Who carried out the research?
The research was carried out by a team of researchers from three universities: City University London in England, and Cardiff and Swansea Universities in Wales. The team was led by Professor Alan Simpson at City University.
Service user and carer involvement:
Of the 13 researchers working directly on the study, six were involved in part time roles as service user researchers: one as co-applicant and the others to interview service users and carers. In addition, there was an advisory group of people with lived experience.
Who funded the research?
The National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (HS&DR 11/2004/12). This is a Government research funding body.
Why did we do the research?
Although there are two different systems in England and Wales, both mean that people receiving mental health services should have a care coordinator, a written care plan and regular reviews of their care. With the introduction of the recovery approach and personalisation, it is now expected that care planning and coordination should be recovery-focused and that people will be taking more control over their own support and treatment.
What were the aims of the research?
We wanted to find out what helps and what hinders care planning for people with mental health problems to be collaborative, personalised and recovery-focused.
By collaborative we mean that care planning is completed in partnership with the service user: the care coordinator works with the service user to plan their care.
By personalised we mean that care is designed with the full involvement of the service user and designed to meet their individual needs.
By recovery, we mean ‘a personal journey … one that may involve developing hope, a secure base and supportive relationships, being more in control of your life and care, social inclusion, how you develop coping skills, and self-management … often despite still having symptoms of mental illness.’
Where was the research carried out?
The research was carried out in six NHS mental health service provider organisations: four in England and two in Wales. One of the reasons for carrying out the research in both England and Wales is that Wales has a legal framework in place called the Mental Health Measure, introduced in 2010. This is intended to ensure that where mental health services are delivered, they focus more appropriately on people’s individual needs. In England, care planning is informed by guidance and is not legally required.
What did we do?
The focus of our research was on community mental health care. We wanted to find out the views and experiences of all of the different people involved: care coordinators (in community mental health teams), managers, senior practitioners, service users and their carers.
- We carried out an extensive literature review.
- We sent out questionnaires to large numbers of people, and received replies from service users (449) and care coordinators (205); these included questions on recovery, therapeutic relationships, and empowerment.
- We interviewed senior managers (12) and senior practitioners (27), care coordinators (28), service users (33) and carers (17).
- We reviewed 33 care plans with the permission of the service users concerned.
What did we find?
Summary of the survey findings:
- There were no major differences between the six sites on the empowerment or recovery scores on the service user questionnaires;
- There were some significant differences between the sites on therapeutic relationships: where there was good collaboration and input from clinicians, relationships were rated as more therapeutic;
- We also found significant differences between sites on some recovery scores for the care coordinators: where they saw a greater range of treatment options, the service was rated as more recovery-focused;
- We found a strong positive correlation between scores on the recovery scale and the therapeutic relationship scale for service users; this suggests that organisations perceived to be more recovery-focused were also perceived as having more therapeutic relationships.
 Mohammad Marie, Aled Jones and I have co-authored a paper arising from Mohammad’s PhD. This appears in the gold open access International Journal of Mental Health Systems, and a copy can be downloaded by following this link.
Mohammad Marie, Aled Jones and I have co-authored a paper arising from Mohammad’s PhD. This appears in the gold open access International Journal of Mental Health Systems, and a copy can be downloaded by following this link. Last Friday afternoon I took the opportunity to visit the
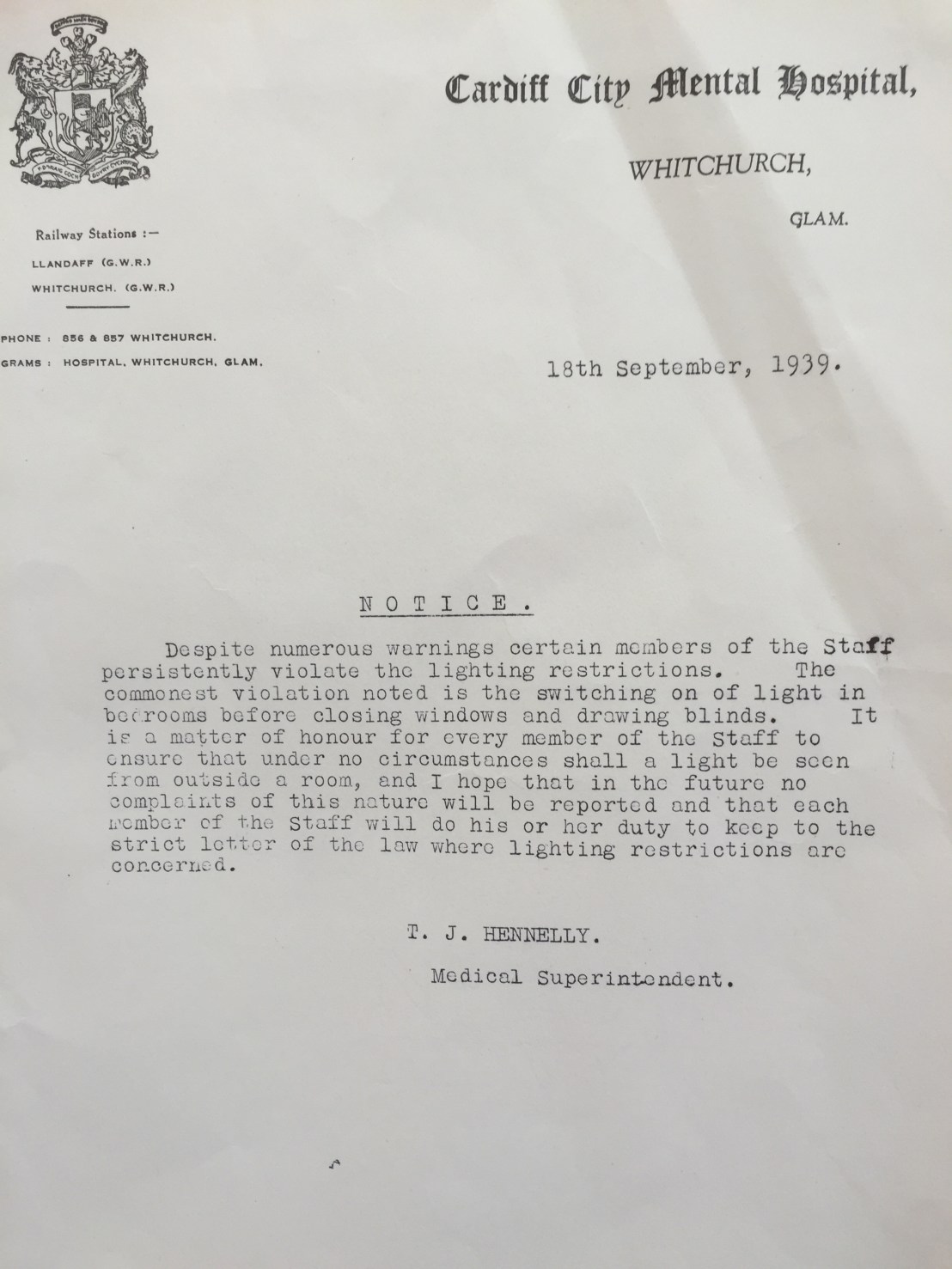
Last Friday afternoon I took the opportunity to visit the 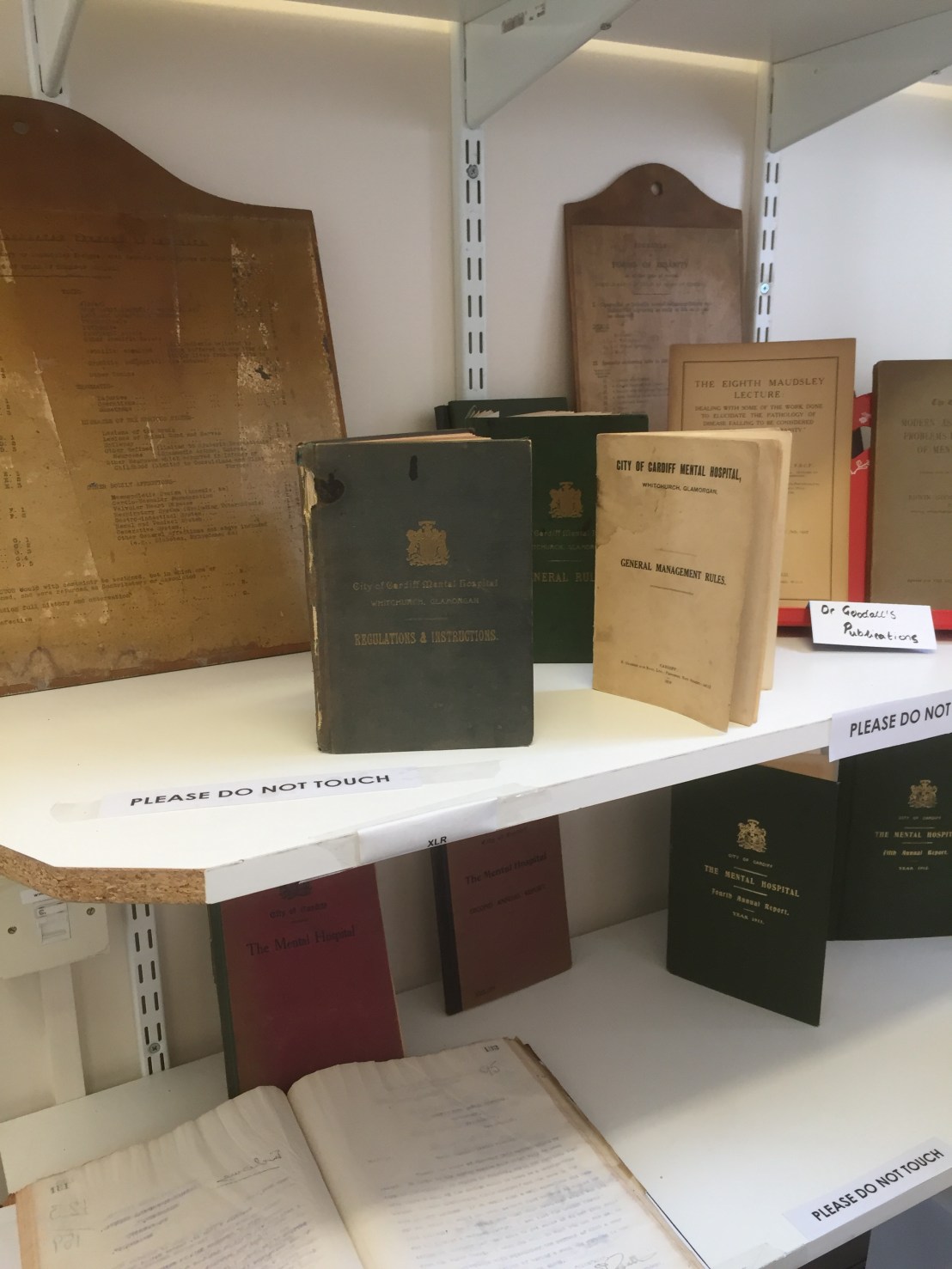


 This morning saw the publication of the
This morning saw the publication of the 
 Lots of interesting things to relate in this post. November 13th saw
Lots of interesting things to relate in this post. November 13th saw  I’ll write more about this in a separate post, but on Thursday November 19th, in
I’ll write more about this in a separate post, but on Thursday November 19th, in 



