Technological failure meant I was unable to participate in this week’s Mental Elf campfire discussion, What has qualitative research ever done for us? The context for the event was the recent decision by the BMJ to reject a paper submitted for publication by members of the McGill Qualitative Research Group on the grounds that qualitative research reports are of low priority. This, the BMJ editors added, is because they are downloaded and cited less often than are reports of quantitative research. The BMJ communication conveying this news to the McGill team was posted on social media, triggering significant protest and then a letter to the BMJ making the case for qualitative methods and urging an editorial rethink.
These kinds of debates over the relative value of different research approaches flare up from time-to-time. Sixteen years ago Philip Burnard and I wrote a paper on the emergence of two camps within mental health nursing. We characterised these with reference to a quantitative/qualitative divide, and made a case for rapprochement and synthesis.
In the event, this week’s campfire which I missed was a sensible and informed one, with excellent speakers. The recording can be viewed here:
For the record, the exemplar piece of qualitative mental health research which I had prepared to talk about is Strauss and colleagues’ Psychiatric ideologies and institutions. I wrote a short piece about this book in 2014, on the occasion of its fiftieth birthday. My view remains that many of the observations made within it are as relevant now as they were in 1964. Ideas and practices, for example, remain contested.
Suffice to say that there has been no shortage of very high-quality qualitative mental health research produced in the years since, including by nurses. Check out these papers by two other invited campfire participants: Alan Simpson on the squeezing of community mental health nurses’ time, and Michael Coffey on the use of time in the accounts of conditionally discharged patients living in the community. Both show how the considered analysis of detailed qualitative data can reveal vital new knowledge of mental health systems, and of the views and experiences of people working within, or using, them. For readers wanting more, over on the Mental Elf website there are currently more than 200 blog posts on recent qualitative research: a rich repository indeed.
This week’s Mental Elf campfire discussion also included some commentary on the use of mixed methods. COCAPP and COCAPP-A demonstrate the value of combining quantitative and qualitative approaches, and reveal how data from surveys, interviews, observations and documentary review can be fruitfully brought together. This type of study is becoming increasingly popular, informed by the idea that different research questions (of a type which might be brought together in a single project) simply require different methods to answer them. This is a position I remain comfortable with.
And so we press on. I’ve been involved in lots of writing lately, as projects yield papers. As per my usual practice, as these appear in journals I’ll aim to write posts on this blog about them and include links to open access versions as I am able. Thanks for reading, and feel free to comment.




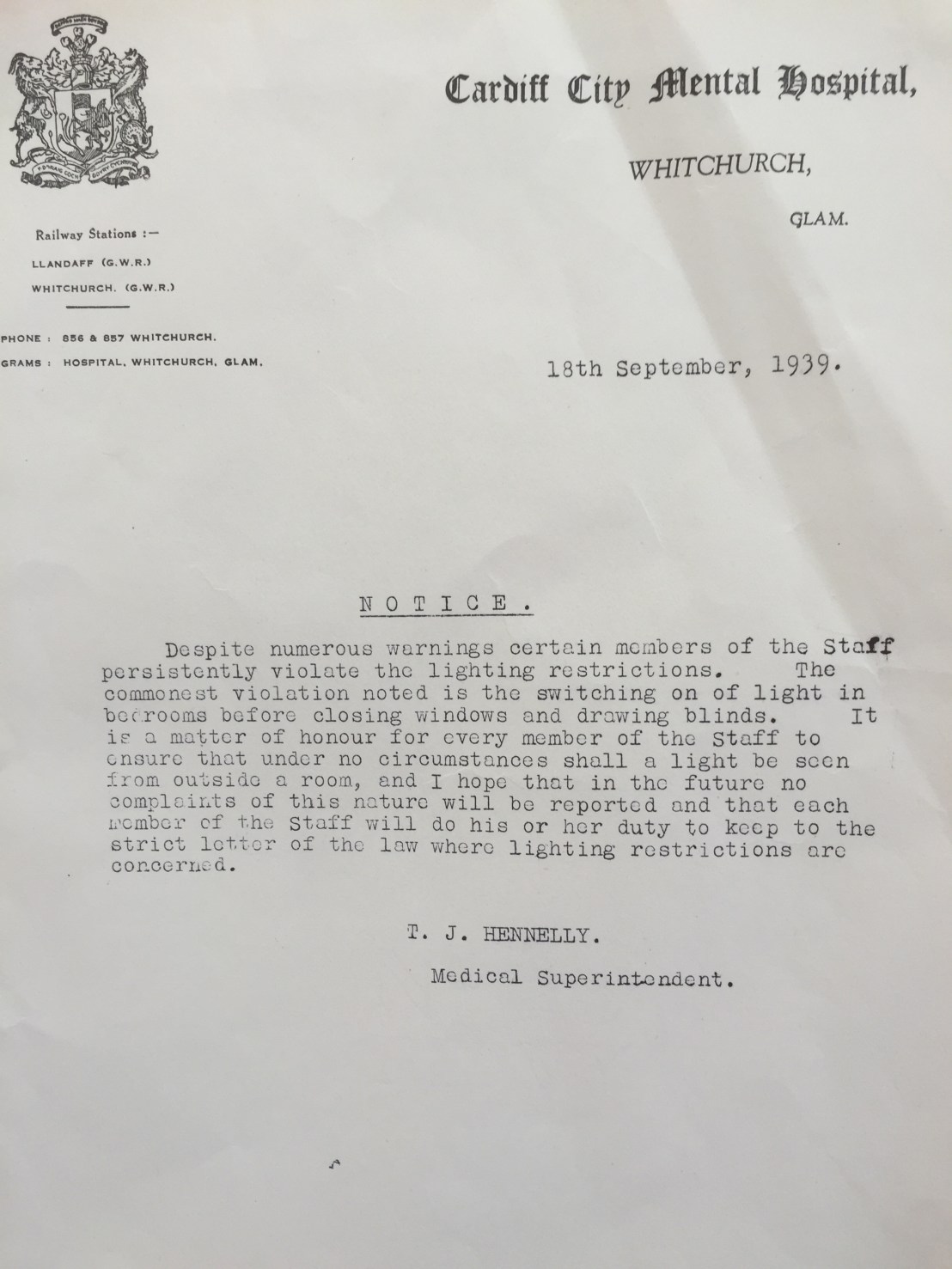
 Last Friday afternoon I took the opportunity to visit the
Last Friday afternoon I took the opportunity to visit the 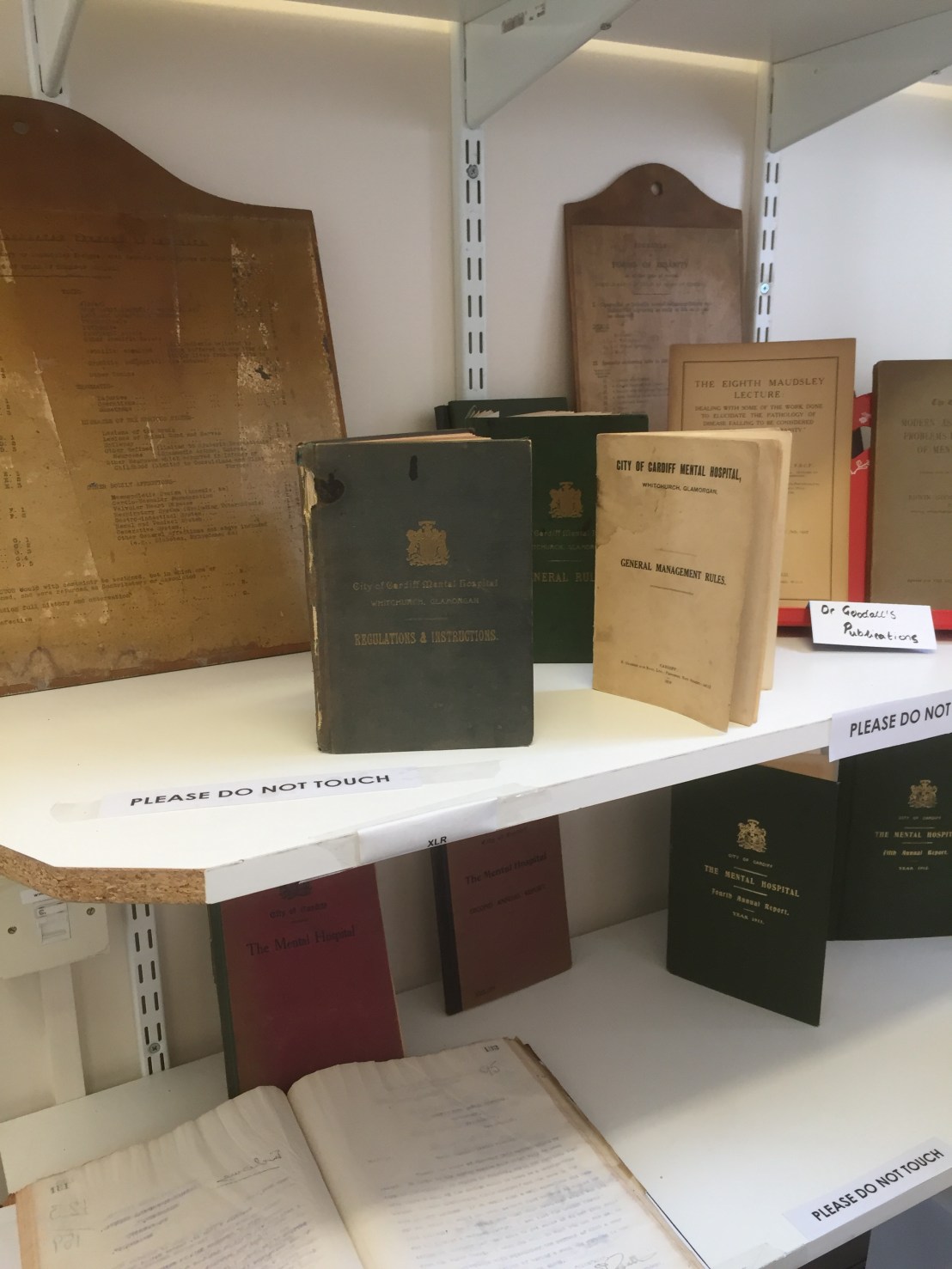


 Over on the
Over on the